
Clinical Data and Supporting Evidence: DECIDE Study
Ceribell Rapid Response EEG was demonstrated to significantly improve clinical accuracy

Results from the DECIDE study (a prospective, multi-center clinical trial to assess Ceribell Rapid Response EEG impact on clinical decision-making) were published in Critical Care Medicine.
Without Ceribell Rapid Response EEG
- Even top academic centers with 24/7 EEG capability have a median 4-hour wait-time for conventional EEG
- Without timely EEG, physicians have to make empiric decisions for treating suspected seizure
Journal Reference
Evaluating the Clinical Impact of Rapid Response Electroencephalography: The DECIDE Multicenter Prospective Observational Clinical Study
Critical Care Medicine. 48(9):1249-1257, September 2020.
Published by: Vespa, Paul M.; Olson, DaiWai M.; John, Sayona; Hobbs, Kyle S.; Gururangan, Kapil; Nie, Kun; Desai, Masoom J.; Markert, Matthew; Parvizi, Josef; Bleck, Thomas P.; Hirsch, Lawrence J.; Westover, M. Brandon Less
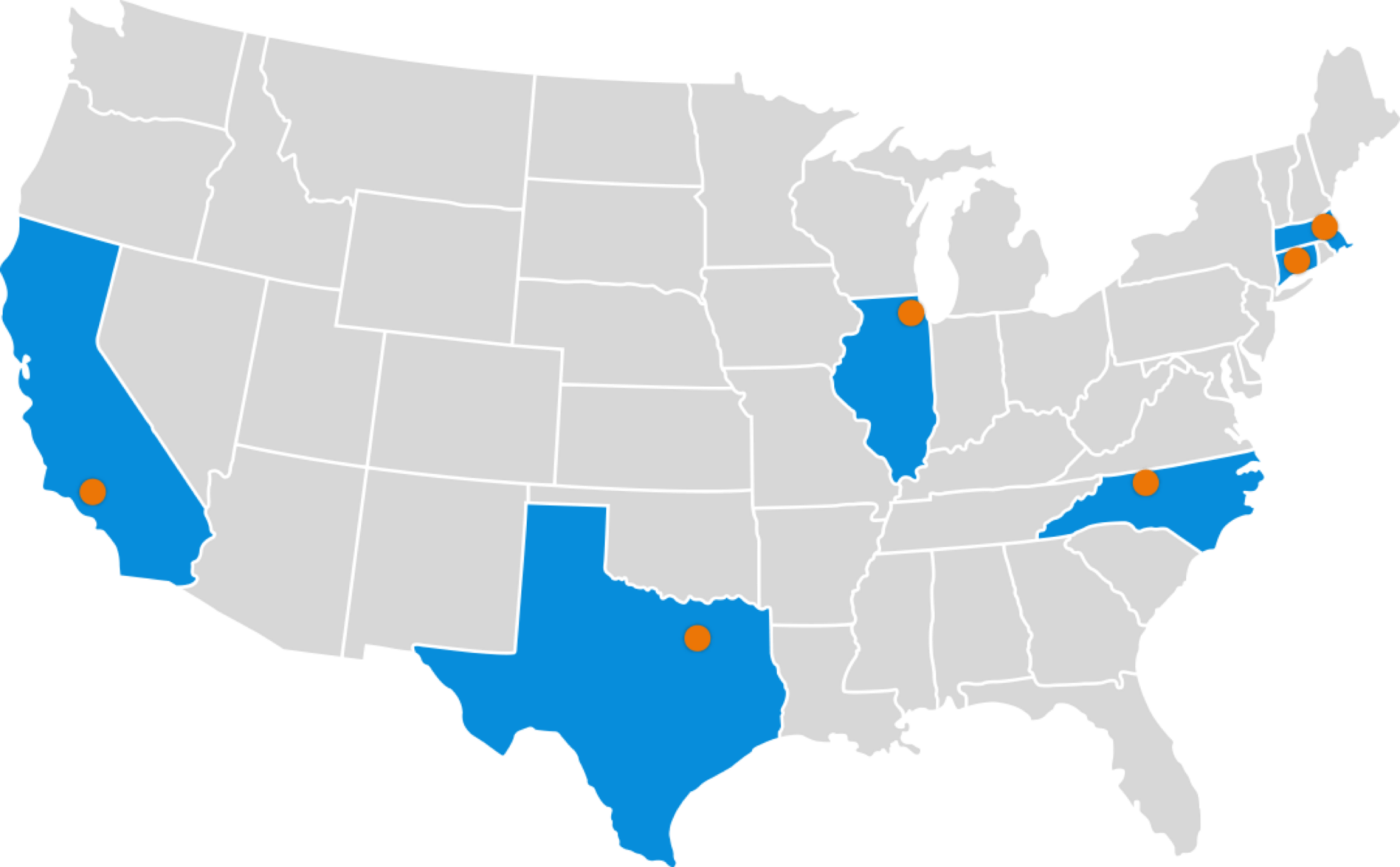
DECIDE Study Design
Prospective, multi-center study conducted at 5 top-tier facilities who had 24/7 EEG access
Investigators
Kyle Hobbs, MD | Wake Forest Baptist Health
Sayona John, MD | Rush University Medical Center
DaiWai Olson, RN, PhD | The University of Texas Southwestern Medical Center
Paul M. Vespa, MD | David Geffen School of Medicine at UCLA
Michael Brandon Westover, MD, PhD | Massachusetts General Hospital
Advisors
Thomas P. Bleck, MD | Rush University Medical Center
Lawrence Hirsch, MD | Yale School of Medicine
The study evaluated 181 patients to assess the performance, timeliness, and ease of use of the Ceribell Rapid Response EEG system in critical care settings
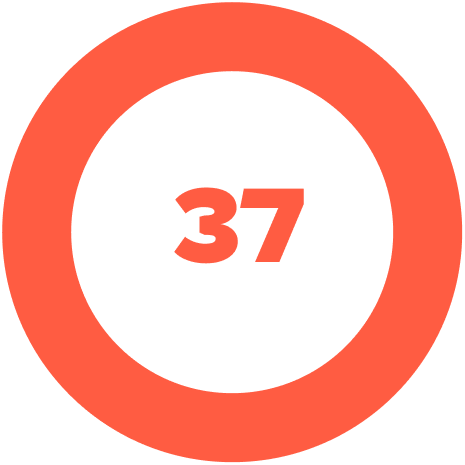
37 bedside physicians
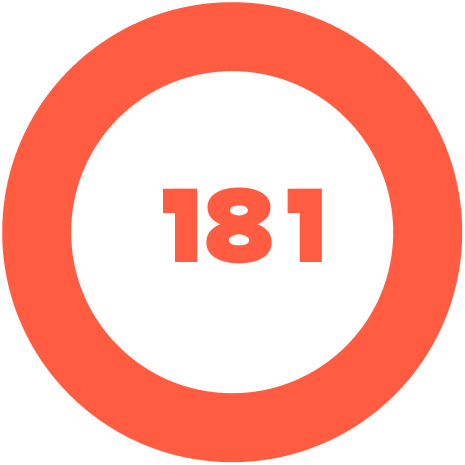
181 patients
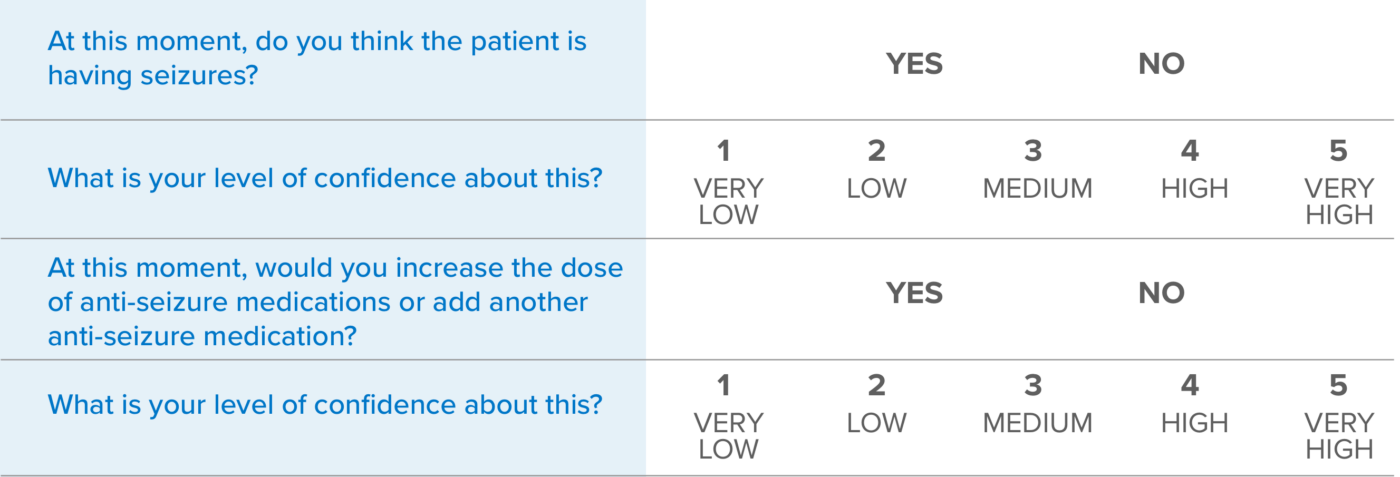
1) Pre-rapid EEG
- Conventional EEG is ordered (time is documented)
- Pre-rapid EEG case form is completed
2) Rapid EEG
- Rapid EEG conducted (time is documented)
- Post-rapid EEG case form is completed
- Rapid EEG is reviewed by 3 epileptologists and classified by majority consensus
3) Conventional EEG
- Conventional EEG arrives (time is collected)
- Conventional EEG recording starts (time is collected)
- Conventional EEG recording is collected
Key Results
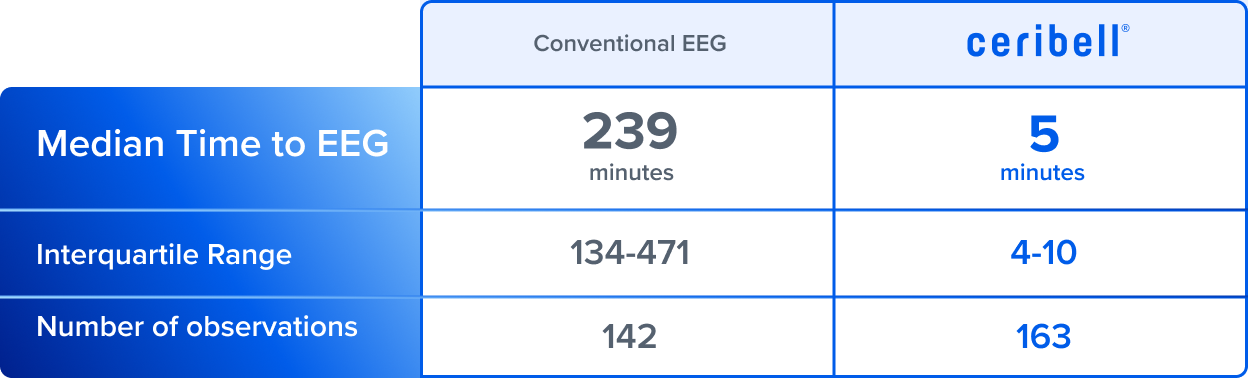
4 hours wait-time to conventional EEG* vs. 5 minutes to Ceribell.
*All but one academic center had at least one on-site EEG tech during after hours
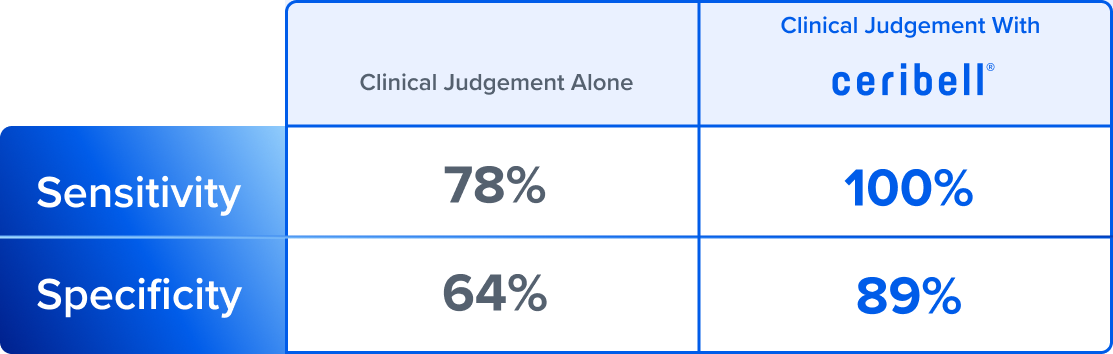
100% sensitivity for detecting seizures with Ceribell* vs. 78% using clinical judgement alone.
*After reviewing Ceribell EEG and using Brain Stethoscope® ;compared to expert neurologist consensus
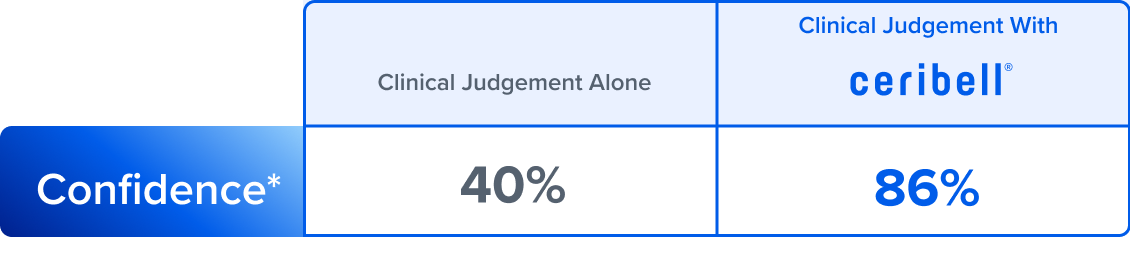
With Ceribell EEG, bedside clinicians rated their diagnostic confidence* high or very high 86% of the time.
*Diagnostic confidence level for each patient reported pre- and post- Ceribell on scale from 1 (very low) to 5 (very high).
Physician and Patient Characteristics
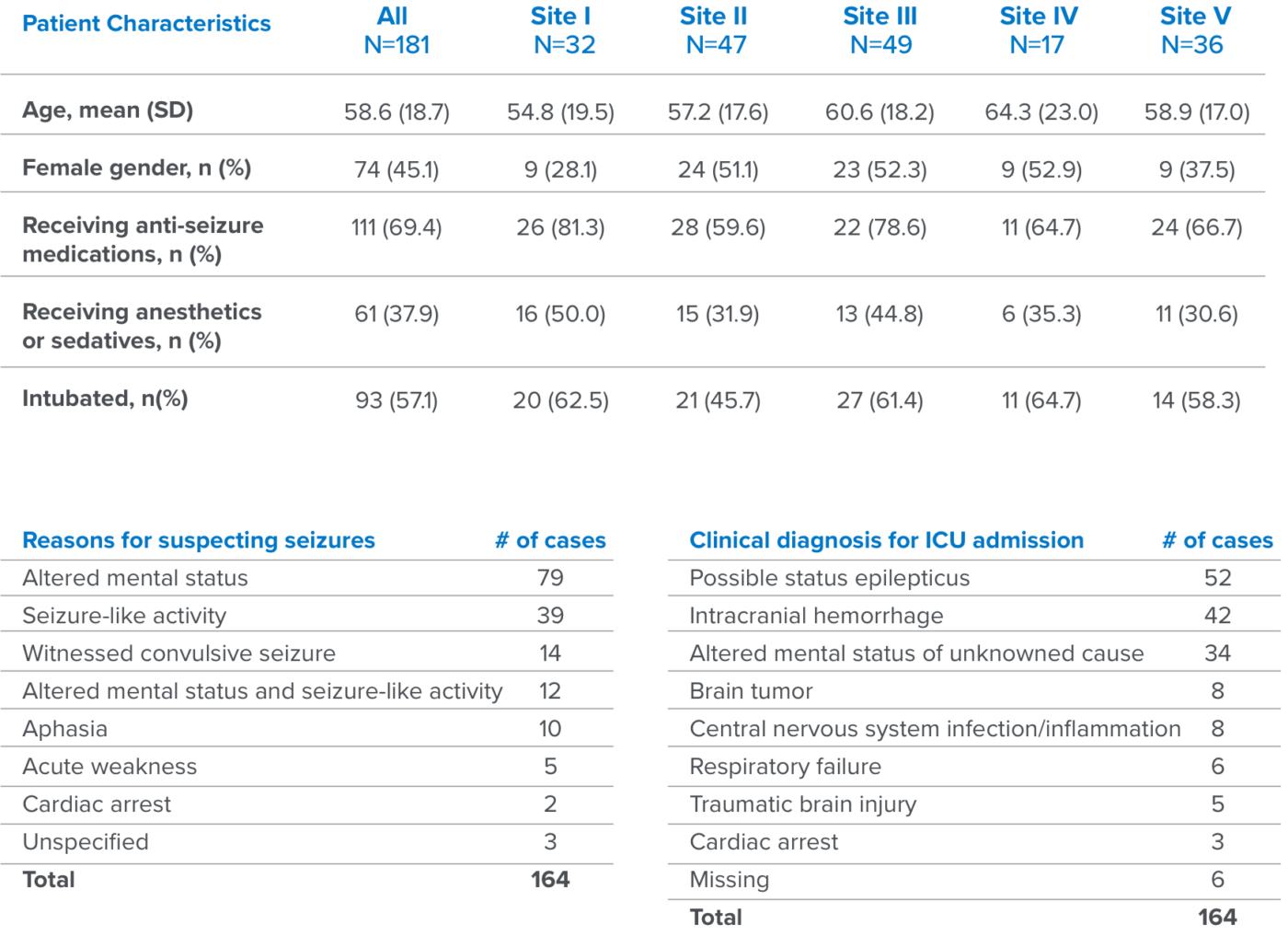
Patient Characteristics
- 181 patients suspected to have non-convulsive seizures for which conventional EEG was ordered were enrolled
- Most patients were already on anti-seizure medications (69%)
- 57% of patients were already intubated
- The majority of patients had some degree of encephalopathy either with or without witnessed seizure or seizure-like activity.
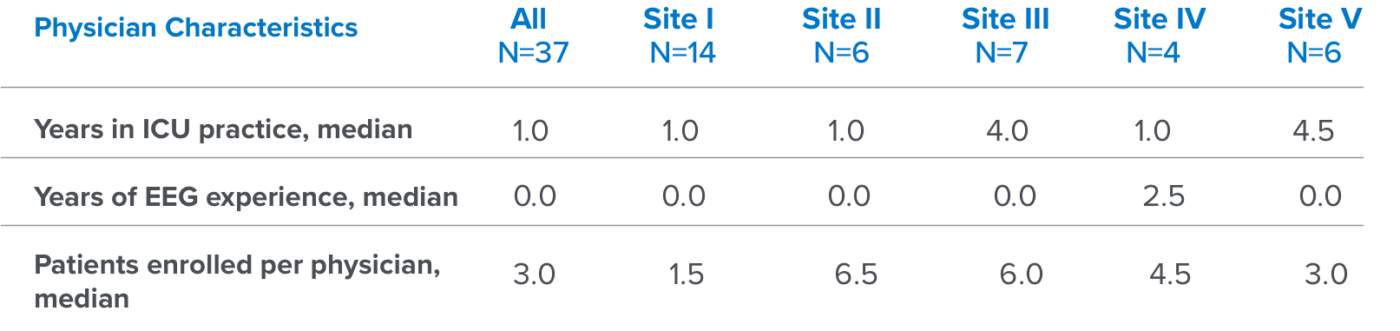
Physician Characteristics
- 37 physicians participated
- All physicians were neurology-trained with varying years of ICU experience and minimal EEG experience

Resources
EEG UNIVERSITY
DECIDE Study Assessing The Impact of Ceribell EEG – Manuscript Review With Dr. Paul Vespa
Watch Our WebinarWebinar
EEG UNIVERSITY