Medical Society Guidelines Emphasize the Need for Prompt EEG Monitoring for Patients at Risk of Status Epilepticus
Given the impact of prompt detection on treatment success and outcomes, medical society guidelines recommend EEG be applied promptly when status epilepticus is suspected and in various conditions in which the risk of status epilepticus is high

“Continuous EEG monitoring should be initiated within 1 h of SE onset if ongoing seizures are suspected.”
NCS Guidelines for Evaluation and Management of Status Epilepticus¹
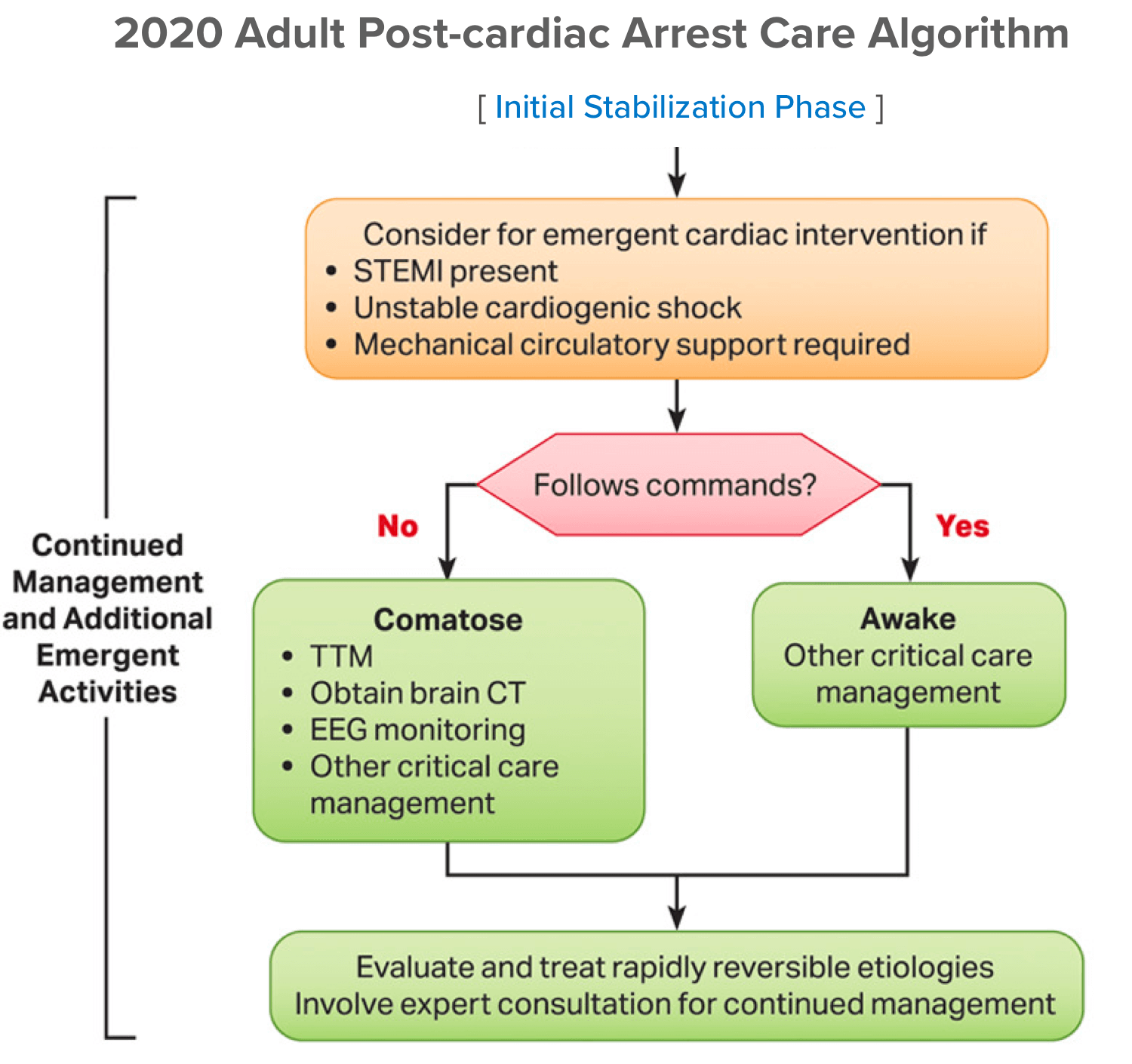
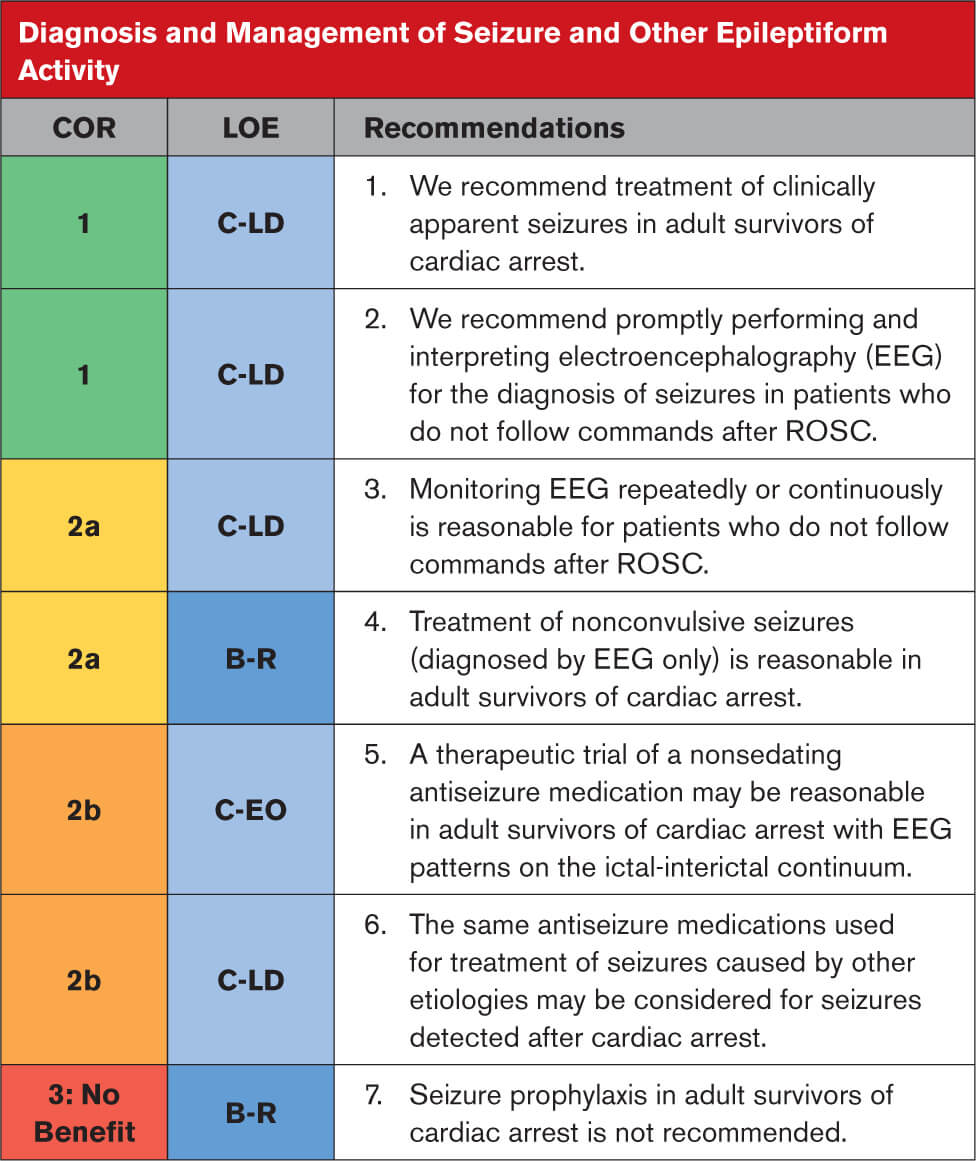
“Recommend promptly performing and interpreting EEG for the diagnosis of seizures in patients who do not follow commands after ROSC.”
AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care²𝄒³

“Growing evidence suggests that [comprehensive post–cardiac arrest care] is critical for both patient survival and optimal neurological outcome.”
R3 Report on Resuscitation Standards for Hospitals⁴

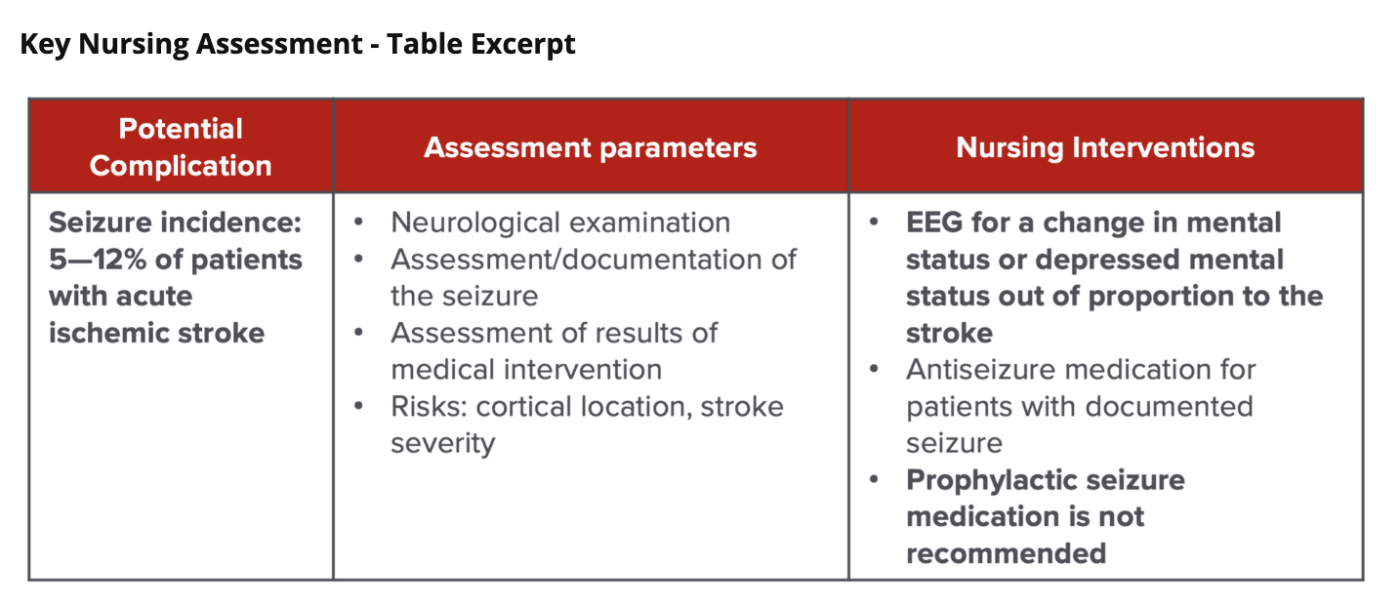
“EEG [is recommended] for a change in mental status or depressed mental status out of proportion to the stroke.”
AHA Comprehensive Nursing Care Scientific Statement for Care of the Patient with Acute Ischemic Stroke⁵

“New-onset seizures in the context of spontaneous ICH are relatively common […] and most of these seizures occur within the first 24 hours of the hemorrhage.”
AHA/ASA Guidelines for the Management of Patients With Spontaneous Intracerebral Hemorrhage⁶

“Monitoring with continuous EEG can detect nonconvulsive seizures, especially in patients with depressed consciousness or fluctuating neurological examination.”
AHA/ASA Guidelines for the Management of Patients With Aneurysmal Subarachnoid Hemorrhage⁷

“CCEEG has an important role in detection of secondary injuries such as seizures and ischemia in critically ill adults and children with altered mental status.”
ACNS Consensus Statement on Continuous EEG in Critically Ill Adults and Children⁸

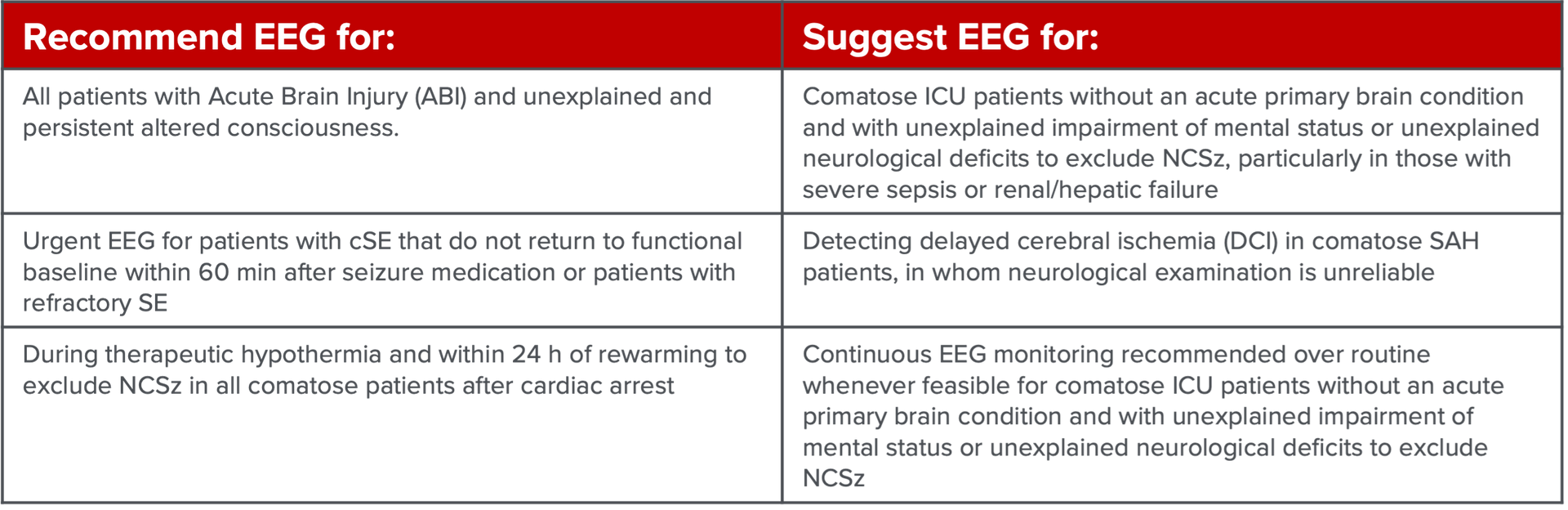
“We recommend EEG in all patients with ABI [Acute Brain Injury] and unexplained and persistent altered consciousness […and] in patients with cSE that do not return to functional baseline within 60 minutes after seizure medication.”
Consensus Summary Statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care⁹
Guidelines and Statements
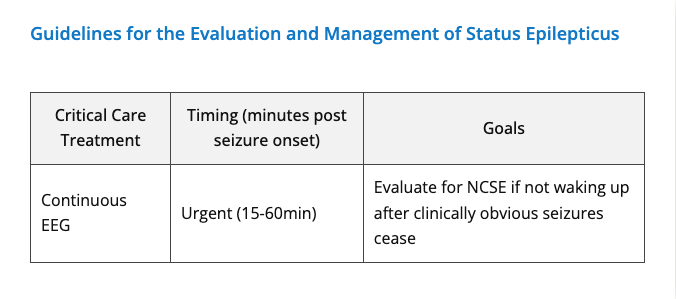
2012 NCS Guidelines for the Evaluation and Management of Status Epilepticus¹
“Continuous EEG monitoring should be initiated within 1 h of SE onset if ongoing seizures are suspected.”

2020 AHA CPR and ECC Guidelines² and 2023 AHA CPR and ECC Guidelines Update³
“Much of post-arrest care focuses on mitigating injury to the brain. Possible contributors to this goal include […] detection and treatment of seizures.”

2022 Joint Commission Requirements, Rationale, and References Report on Resuscitation Standards for Hospitals4
“The Joint Commission technical advisory panel on resuscitation and the 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care strongly recommended the implementation of comprehensive, structured, and multidisciplinary protocols of care to optimize survival and neurological outcome.”
“Comprehensive post–cardiac arrest care is necessary to address the systemic effects of the ischemia-reperfusion injury following cardiac arrest. Growing evidence suggests that it is critical for both patient survival and optimal neurological outcome.”
![]()
2021 AHA/ASA Comprehensive Nursing Care Scientific Statement for Care of the Patient with Acute Ischemic Stroke5
“Neurological complications, including […] poststroke seizures result in early neurological deterioration, associated with poor outcomes.”
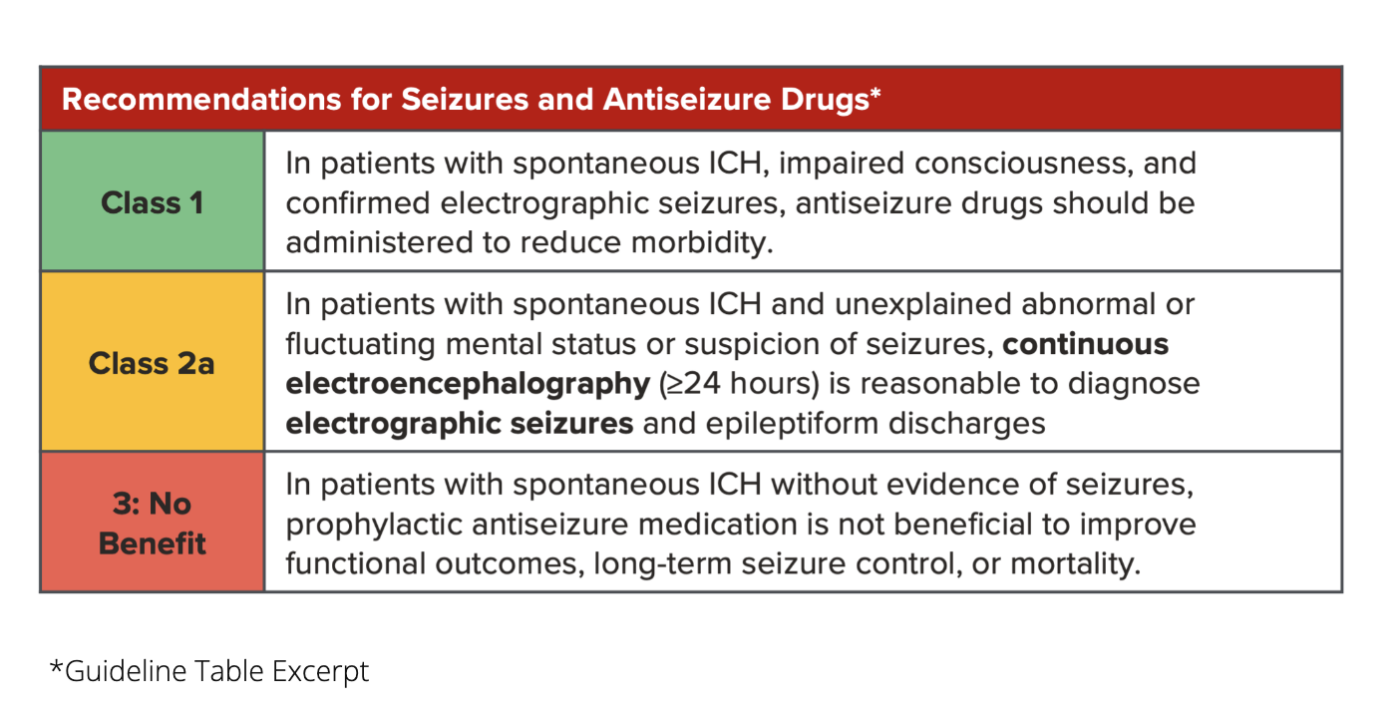
2022 AHA/ASA Guideline for the Management of Patients with Spontaneous Intracerebral Hemorrhage6
“New-onset seizures in the context of spontaneous ICH are relatively common […] and most of these seizures occur within the first 24 hours of the hemorrhage.”
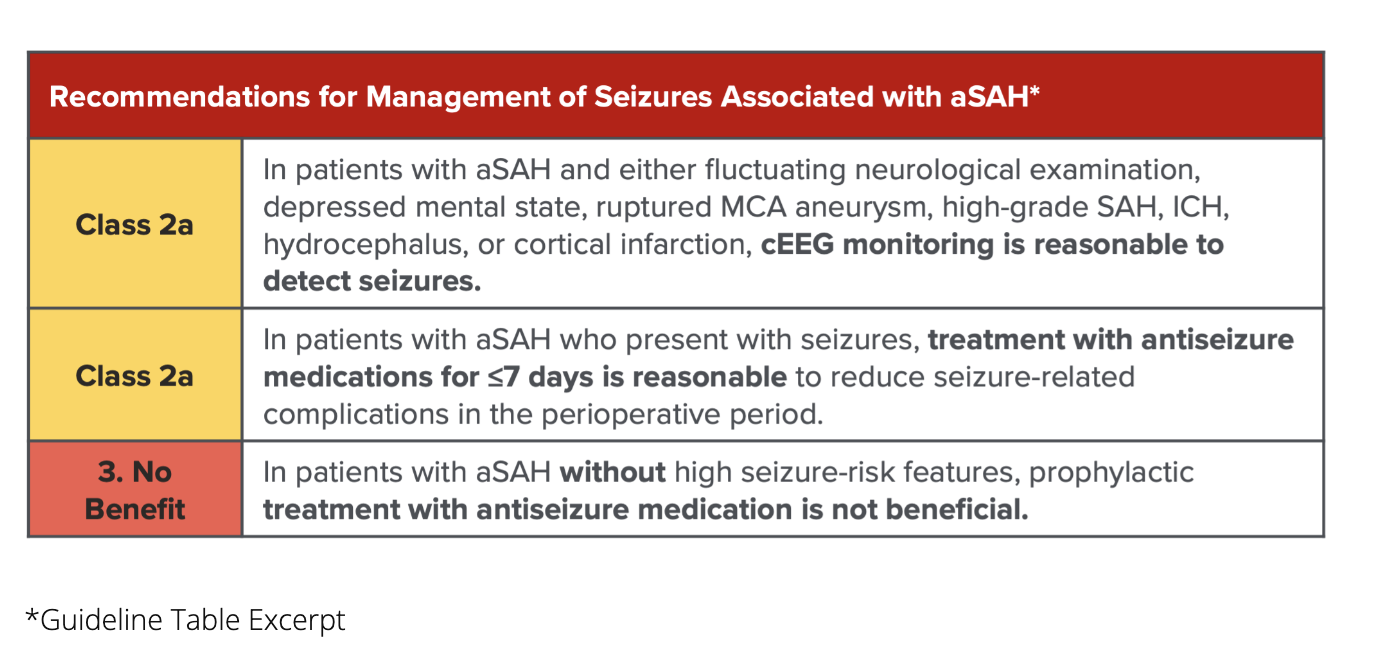
2023 AHA/ASA Guideline for the Management of Patients With Aneurysmal Subarachnoid Hemorrhage7
“Monitoring with continuous EEG can detect nonconvulsive seizures, especially in patients with depressed consciousness or fluctuating neurological examination.”
![]()
2015 ACNS Consensus Statement on Continuous EEG in Critically Ill Adults and Children8
“CCEEG has an important role in detection of secondary injuries such as seizures and ischemia in critically ill adults and children with altered mental status.”

2014 NCS Consensus Summary Statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care9
“We recommend EEG in all patients with ABI [Acute Brain Injury] and unexplained and persistent altered consciousness […and] in patients with cSE that do not return to functional baseline within 60 minutes after seizure medication.”
Other Resources
2024 CNSA Clinical Proceedings on Nonconvulsive Status Epilepticus10
“Rapid diagnosis and treatment of status epilepticus is critical because if not promptly treated, status epilepticus can swiftly evolve into a self-sustaining condition, and become resistant to benzodiazepines and other antiepileptic medications.”
“With a shortage of EEG technicians and limited resources, rapid EEGs coupled with 2HELPS2B can aid in stratifying seizure risk.”
