A Sampling of Clinical Data and Supporting Evidence
The Ceribell EEG system has been clinically validated across 135+ publications and abstracts, including reports on 2 multi-center trials
Impact on Clinical Management
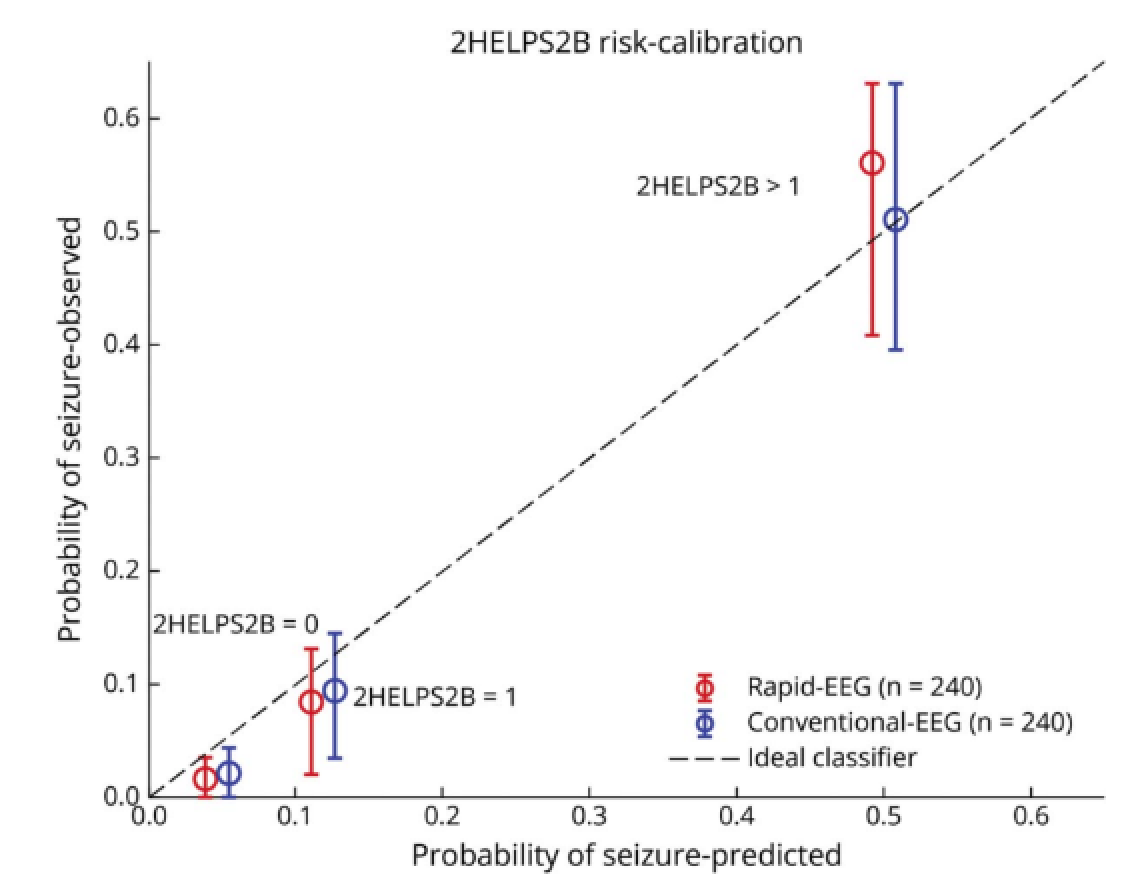
SAFER-EEG TRIAL: Performance of the 2HELPS2B score with Ceribell is comparable to conventional EEG for forecasting seizure risk in acutely ill patients1
A retrospective multi-center study that enrolled over 1000 patients who were monitored by EEG during their stay from January 1, 2018, to June 20, 2022. For the primary analysis, 240 Ceribell EEG patients* and 650 conventional patients* were included and matched for confounders to evaluate the feasibility of using Ceribell EEG to assess future seizure risk at the hospital. Estimated 2HELPS2B score for seizure-risk forecasting based on the 1st hour of EEG.
- Comparable 72 hours in-hospital seizure risk forecasting with Ceribell vs. conventional EEG
- If Ceribell 2HELPS2B=0, the risk of seizures in the next 24h is only ~2%
*patient’s EEG was determined by the first EEG they received during hospital visit
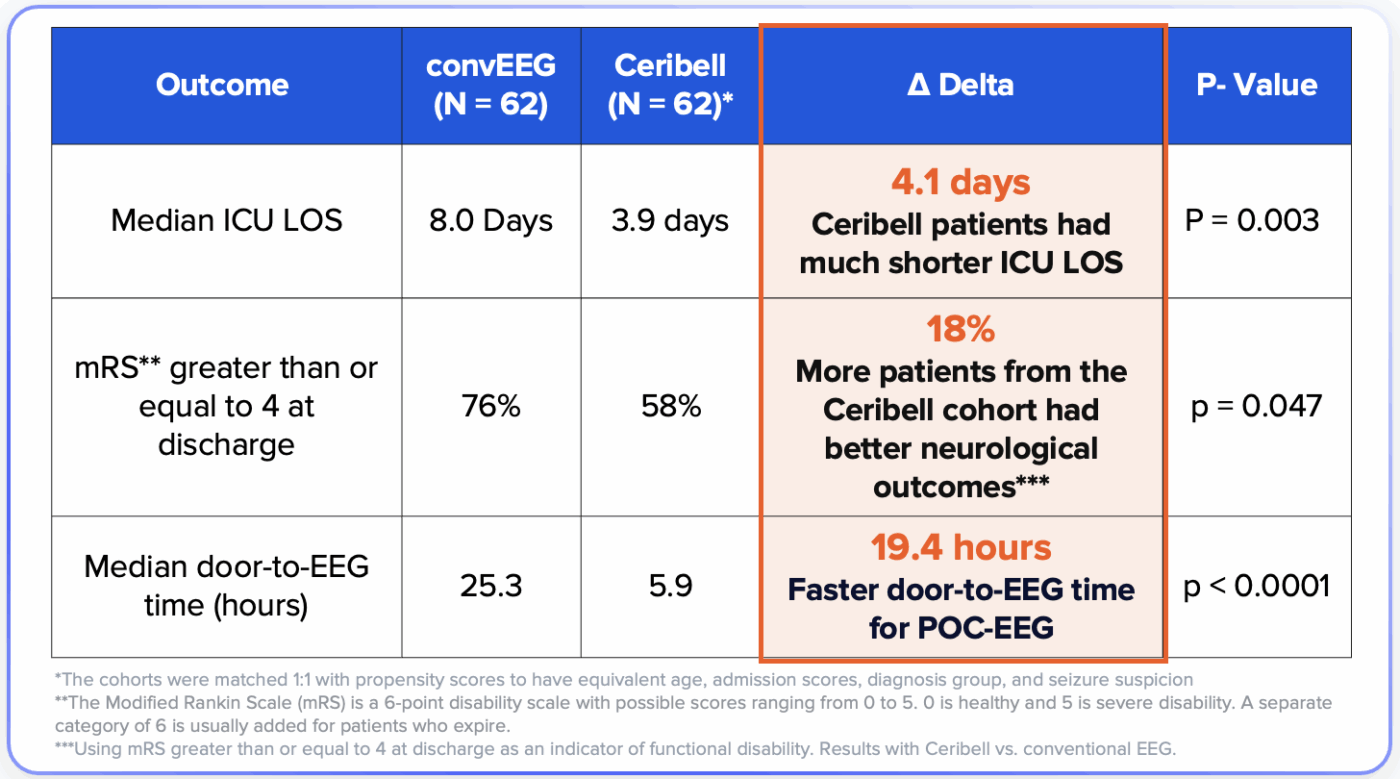
SAFER-EEG TRIAL: Shorter median ICU length of stays with Ceribell and more patients from the Ceribell cohort with better neurological outcomes compared to conventional EEG2
- 4.1-day shorter median ICU length of stay with Ceribell vs. convEEG
- 18% more patients from the Ceribell cohort had better neurological outcomes***
- 19.4 hours faster door-to-EEG time
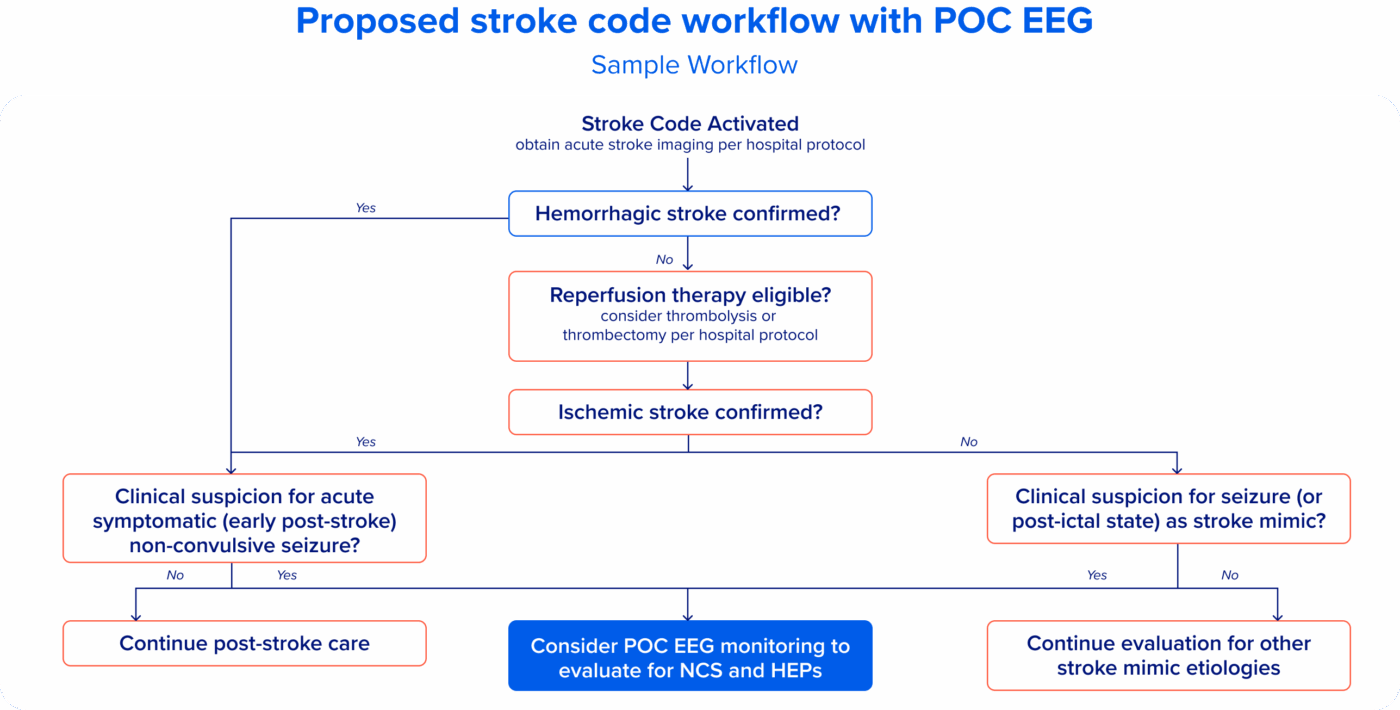
POC EEG has the potential to help expedite diagnosis of non-convulsive seizures masquerading as stroke during acute stroke evaluation, or during the acute post-stroke phase when seizures are prevalent.3
A sub-analysis of stroke-code patients from a retrospective study conducted at Providence Mission Hospital, a large tertiary-care community teaching hospital. The authors assessed 70 patients who underwent Ceribell point-of-care EEG monitoring during or closely following stroke code activation.
- 1/3 of stroke mimic patients had seizures or HEP*
- 16% of confirmed stroke patients had seizures or HEP*
- Based on the results of the sub-analysis, the study suggests the use of Ceribell POC EEG under the proposed workflow
*highly epileptiform patterns
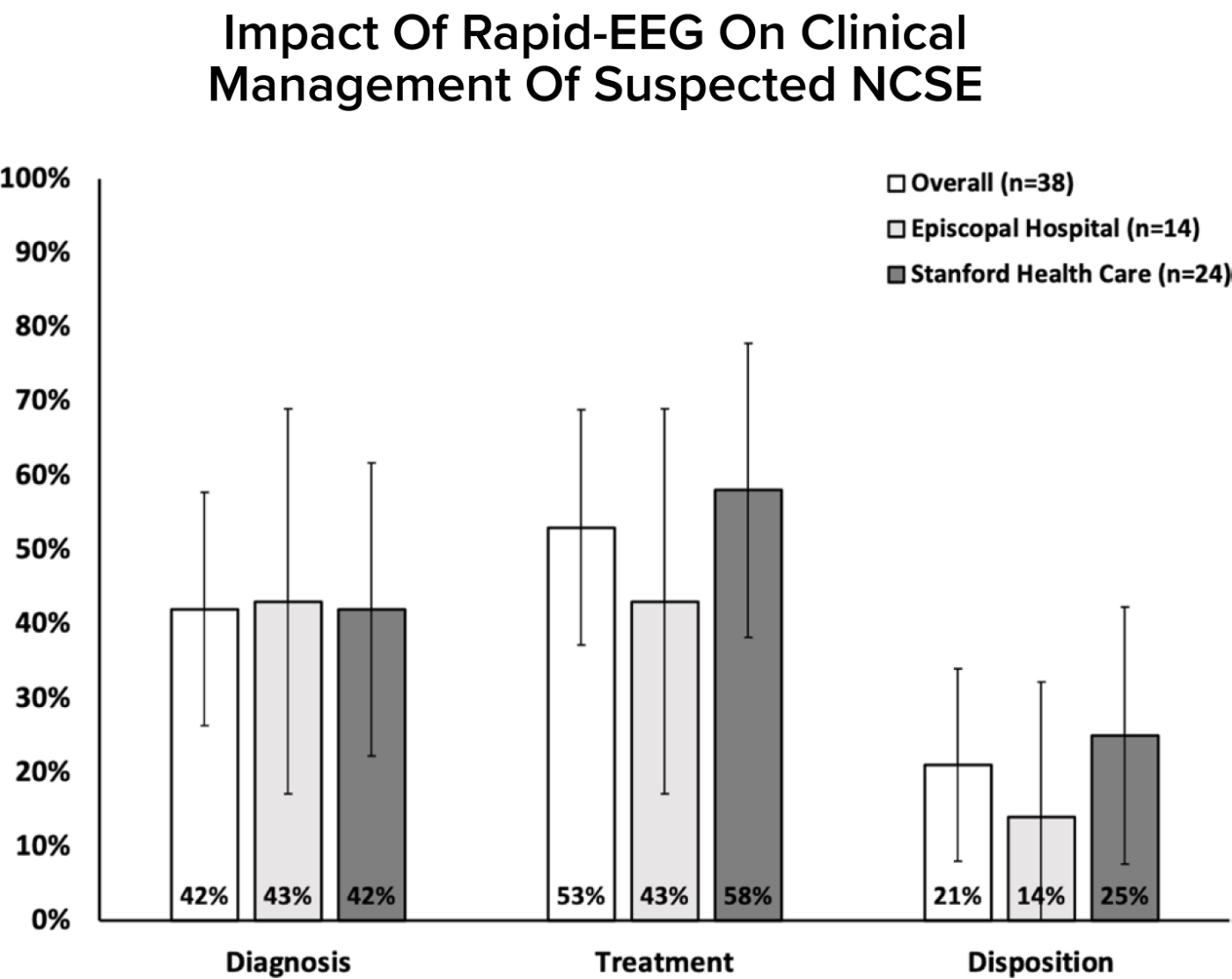
Ceribell use in the ED has the potential to positively impact the clinical management of suspected non-convulsive seizures4
This prospective study conducted at two ED sites evaluated rapid EEG impact on seizure management when used by emergency physicians. Ceribell changed clinical management for 53% of patients.
- Ceribell expedited disposition of 21% of patients
- ED physicians identified seizures with 100% sensitivity and 92% specificity when using Brain Stethoscope
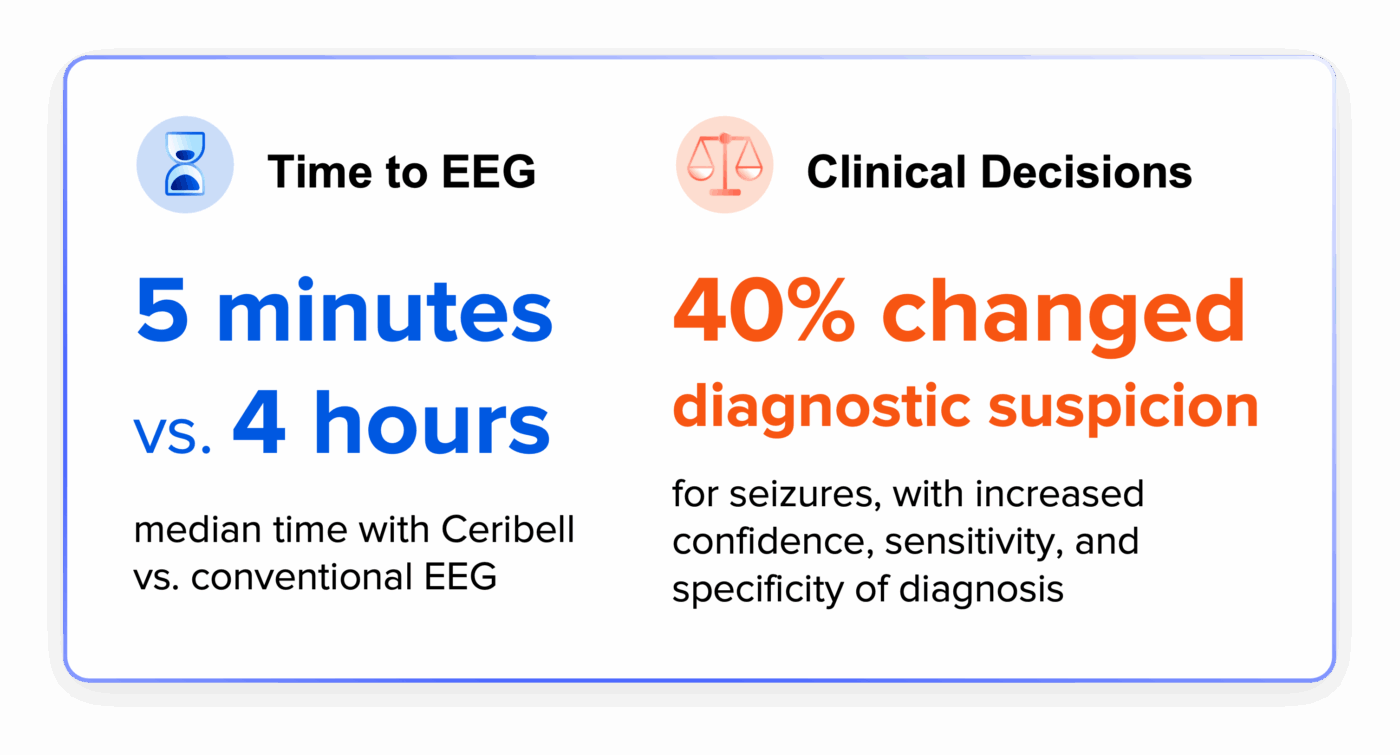
DECIDE TRIAL: Ceribell Point-of-Care EEG was demonstrated to significantly improve clinical accuracy and confidence5
The DECIDE trial was a prospective, multi-center observational study that evaluated the clinical impact of Point-of-Care EEG. The device was set up by neurology residents and fellows without prior experience with Ceribell EEG. The qualitative results came from evaluations in user surveys.
Clarity Performance

Ceribell with Clarity offers 24/7 EEG monitoring with consistently high performance for detecting non-convulsive status epilepticus6,7
Retrospective assessment of clinical Ceribell EEGs across 10+ centers evaluated the performance of Clarity to epileptologist consensus in generating bedside alerts for possible status epilepticus.
- 95% Sensitivity for alerting to suspected status epilepticus*
- 97% Specificity for ruling out status epilepticus*
- 99.9% NPV for ruling out seizure and status epilepticus**
*At ≥ 90% seizure burden
**At 0% seizure burden
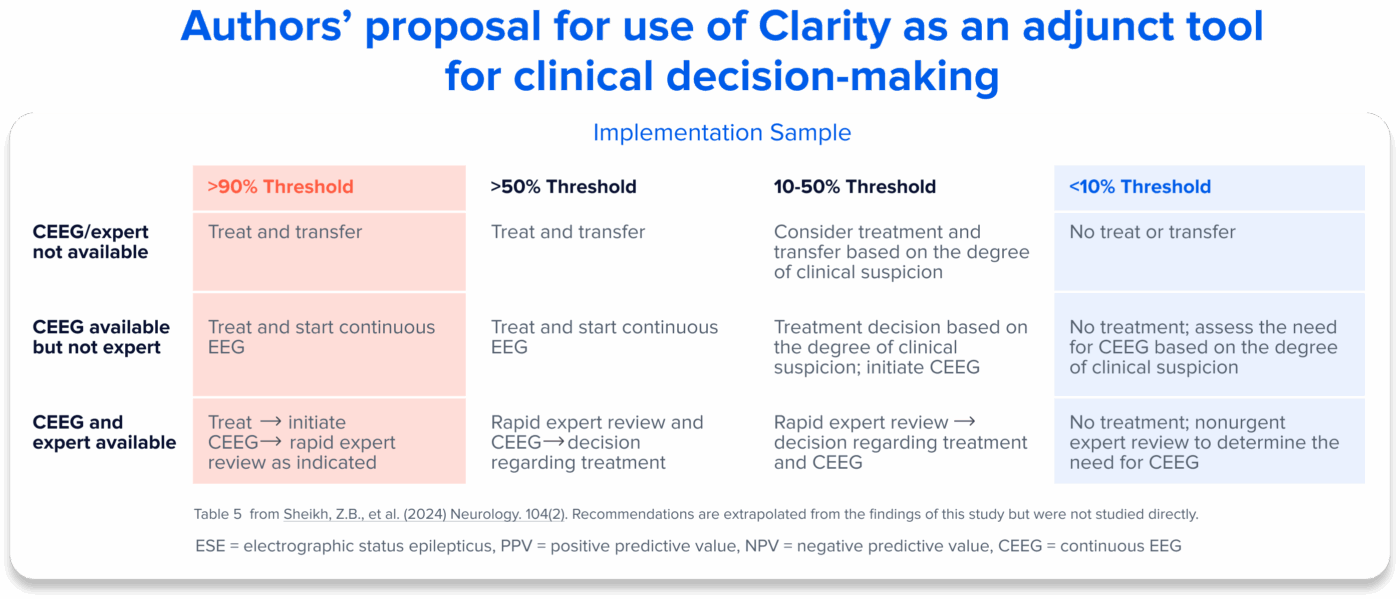
AccuRASE Study: An independent study from Yale, published in Neurology as Level II evidence, reinforces the clinical value of Clarityv68
A retrospective study of 235 sequentially sampled, deidentified Ceribell EEGs from the Yale New Haven Health System (2 community hospitals and 1 tertiary care center). Groups of 3 out of 12 total expert clinical neurophysiologists blinded to the Clarityv6 output and clinician notes, read subsets of Ceribell EEGs. Studies were reviewed and labelled as ESE or possible ESE (pESE) where relevant, per 2021 ACNS guidelines.
- At 90% seizure burden threshold*, Clarityv6 detected ESE/pESE with 99% SPECIFICITY and 78% PPV
- At 10% seizure burden threshold*, Clarityv6 detected ESE/pESE with 88% SENSITIVITY and 98% NPV
*These outcomes were evaluated at seizure burden (SzB) thresholds: >1%, >10%, >20%, >50%, and >90% compared to the expert determination described in Key Results.
Health Economics
Ceribell EEG is Associated with Improved Patient Care and Increased Reimbursement9
Retrospective 6-month review after POC EEG QI protocol implementation, compared to 6 months prior to POC EEG acquisition.
- 3-day trend of shorter median LOS, resulting in ~$4,850 average cost savings per patient
- 13% of Ceribell patients qualifying for seizure-associated CC or MCC reimbursement, leading to ~$7,300 average additional payment
Ceribell Point-of-Care EEG has the potential to alter the treatment course for patients with suspected seizures and may result in cost savings per patient10
This study built a two-armed cost–benefit model comparing decisions based on rapid EEG results with those based on clinical suspicion alone to examine the potential effect of Ceribell on hospital costs.
- Rapid EEG savings were $5,633 per use case (95% PI: $4,649 to $6,617)
- Cost savings were demonstrated in 75% of replications
- 64% of variance in total costs was attributable to LOS for patients incorrectly diagnosed with seizures
Signal Quality
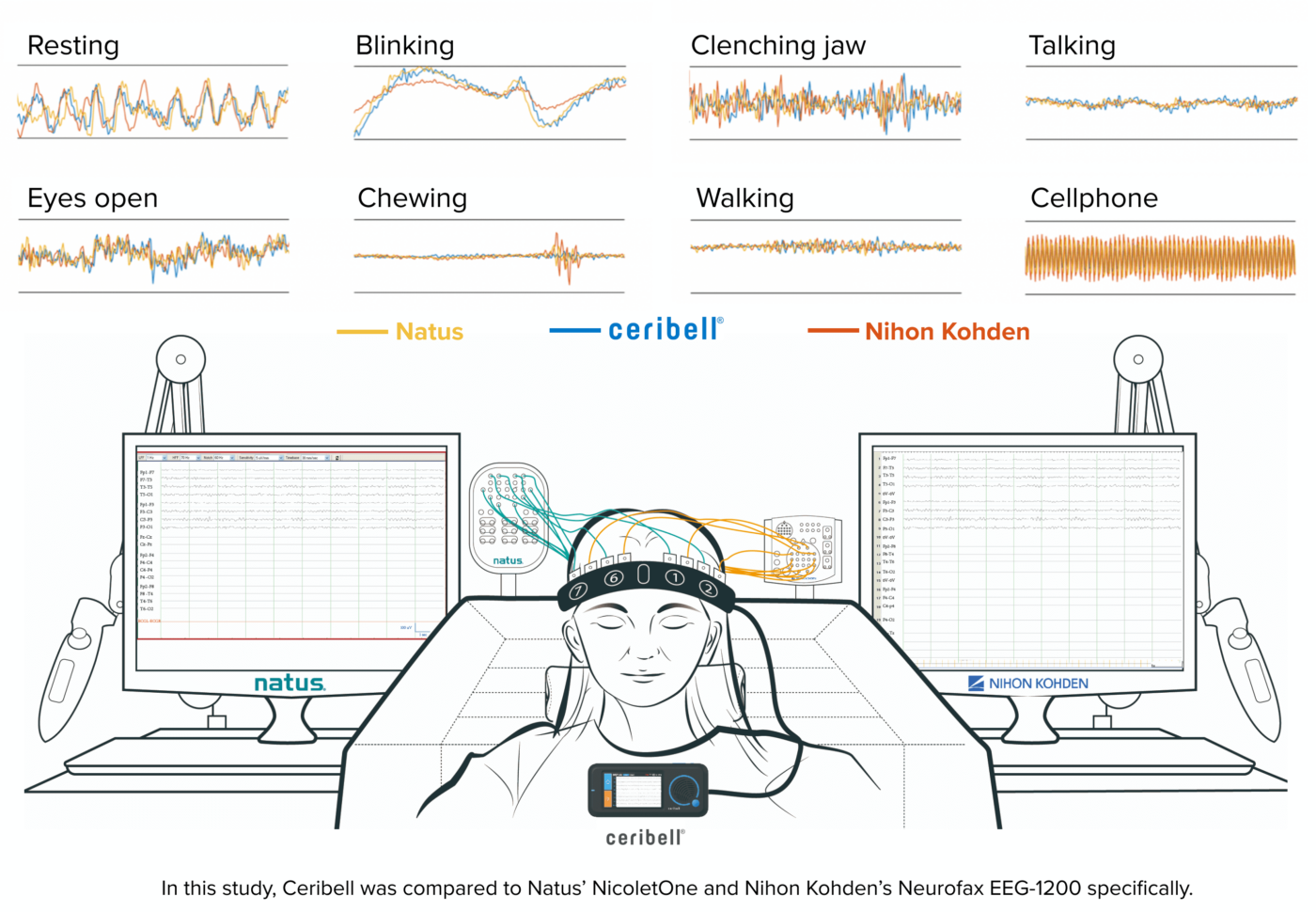
Ceribell EEG offers equivalent signal quality to conventional EEG13
Ceribell was compared to Natus and Nihon Kohden in three-way simultaneous recordings and demonstrated equivalence. Ceribell was also compared to conventional systems in consecutive recordings, demonstrating equivalence for all quality metrics apart from noise, where Ceribell had significantly lower 60 Hz noise.

Resources
In The News
In The News
DECIDE Study Assessing The Impact of Ceribell EEG – Manuscript Review With Dr. Paul Vespa
Watch Our WebinarWebinar