
The Challenge of Non-Convulsive Status Epilepticus
NCSE is a neurological emergency that needs to be treated quickly to prevent brain damage. An electroencephalogram (EEG) is required to detect these seizures, but conventional EEG systems are not optimal for acute care needs
Prevalence
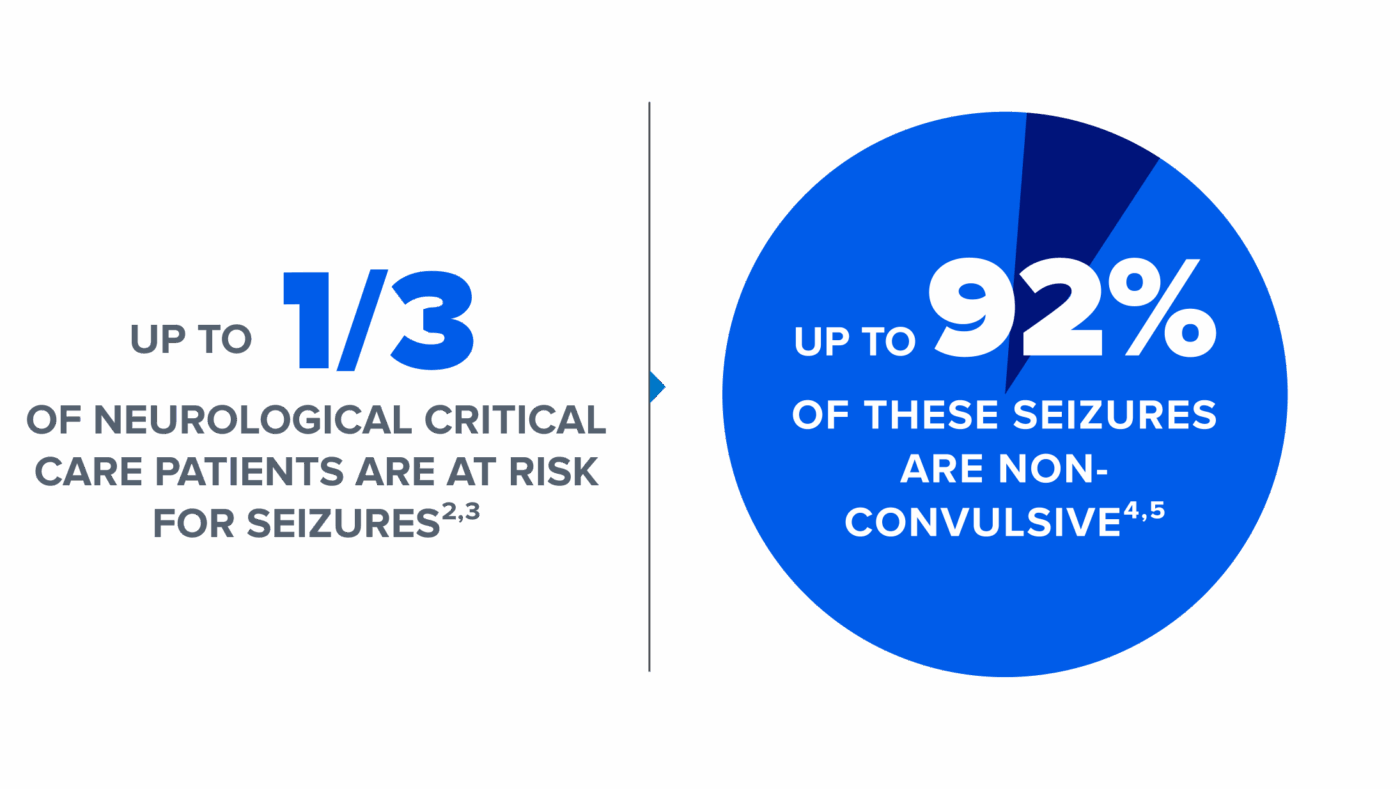
Non-convulsive seizures, including cases of non-convulsive status epilepticus (NCSE), are common in critically ill patients in emergency departments and intensive care units.1
Diagnosis

- Prolonged seizure activity, starting at 5 minutes, may lead to a condition known as status epilepticus, which can have long-term neurological consequences depending on the type and duration of the seizures.6
- Patients with non-convulsive status epilepticus lack the physical symptoms7 that are often used to identify seizure activity, which makes empirical diagnosis extremely challenging.
- Prompt detection and treatment of non-convulsive status epilepticus is crucial for reducing likelihood of poor outcomes.6
Guidelines and Statements

“Continuous EEG monitoring should be initiated within 1 h of SE onset if ongoing seizures are suspected.”
“Recommend promptly performing and interpreting EEG for the diagnosis of seizures in patients who do not follow commands after ROSC.”
“EEG [is recommended] for a change in mental status or depressed mental status out of proportion to the [ischemic] stroke.”
“Monitoring with continuous electroencephalography can detect nonconvulsive seizures, especially in patients with depressed consciousness or fluctuating neurological examination.”
Clinical Reality: Conventional EEG is Not Suited for Critical Care

EEG services often rely on a few key personnel, which makes emergency requests difficult – especially after hours. Bedside clinicians are often left with three unappealing choices – wait for an EEG test, treat the patient empirically, or transfer the patient to a better equipped facility. None of these choices is appealing to clinicians, as each could result in poor clinical outcomes for the patient as well as impose cost burdens on the hospital and payers.

CURRENT EEG PRACTICE:
-
Conventional EEG systems require set up by specialized EEG technicians who typically work limited hours and are in short supply nationally.
-
Conventional EEG systems consist of large and cumbersome capital equipment which is generally not stored in the acute care setting.
-
The setup process is long, complex, and labor-intensive, taking up to 30 minutes to complete.
-
The recording must be interpreted by specially trained neurologists, who are also in short supply.
-
EEG interpretation is a complicated and time-consuming task, and neurologists are not always immediately available to interpret urgent EEG requests.
The combination of these factors can result in multi-hour, or even multi-day, delays in EEG administration and interpretation in the acute care setting.
Dr. Bleck discusses the importance of rapidly applying EEG to obtain a diagnosis and treat non-convulsive status epilepticus quickly
“Unless you do an EEG of some sort, you don’t know. We should really be attaching an EEG to the patient very quickly.”
DR. THOMAS P. BLECK
Founding President of Neurocritical Care Society

Resources
Webinar
Webinar
Webinar